SJS is an acute, rare and potentially dangerous skin reaction that requires hospital administration.. It usually involves skin, mucus membrane, accompanied by systemic symptoms.
Most prevalent cause of its occurrence, nearly in 80 % of cases are medication, either sensitivity reaction or overdose reaction.
SJS is very nearly similar to Toxic Epidermal Necrolysis (TEN), which is an even more severe form of SJS. SJS and TEN are basically distinguished on the basis of extent of area of skin detachment.
CAUSES-
SJS is usually an unpredictable condition, which may be triggered by any medication, infection or both. Symptoms of SJS tend to appear while a person is on that particular medication and even after 2 weeks of termination of that particular medication.
Medications that are known to causeSJS in some sensitive patients are-
Pain killers, such as acetaminophen (Tylenol, etc), ibuprofen (Advil, Motrin IB, etc) and naproxen sodium (Aleve)
Antibacterial sulfonamides ( sulfasalazine), penicillins, cephalosporins, quinolones, minocycline
Paracetamol/acetaminophen
Medicines for treating epilepsy (anticonvulsants) or mental illness (antipsychotics)Anti-gout medication (alloprinol), etc
Infections that can cause Stevens-Johnson syndrome include pneumonia and HIV.
HISTORY AND PROGRESS OF SYNDROME-
Patients complain of non-specific symptoms in the initial phase of reaction, like- fever, malaise, URTI ( causing - sore eyes, cough, rhinitis, myalgia, etc). Which usually go unnoticed and patients usually do not relate it to medicinal reaction and continue to take that triggering medication.
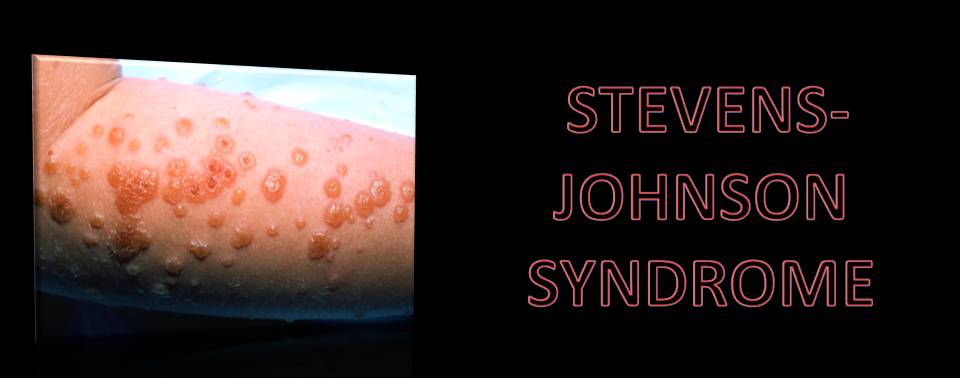
After 3 days or so, painful rashes that change to blistering rashes start appearing, covering - face, neck, trunk, limbs and mucosal membranes of mouth (including lips), pharynx, oesophagus, GIT, genitals, upper respiratory tract, etc.
The blisters then merge to form sheets of skin detachment, exposing red, oozing dermis. The Nikolsky sign is positive in areas of skin redness (blisters and erosions appear when the skin is rubbed gently).
NOTE- SJS and TEN are distinguished at this stage by appearance of targetoid rashes, and fewer area of denudation in SJS; while widespread tender erythroderma and erosion in TEN
The patient is very ill, anxious, and in pain. Liver, kidneys, lungs, bone marrow, and joints may be affected by Stevens-Johnson syndrome/toxic epidermal necrolysis.
After a week or so, blisters start rupturing, leaving a nude lesion behind, which demands extra care for the risk of catching superadded infection.
DOES THIS NEED URGENT MEDICAL ATTENTION?
A big YES!!!! SJS and TEN require emergency medical attention and care.
RISK FACTORS-
SJS and TEN is most likely to occur in patients with history of-
HIV infection increases risk of SJS by 100 fold.
Weak immunity
Cancer, especially blood cancer.
Personal or family history of SJS.
BASIC MANAGEMENT-
Cessation of suspected and proved medicine.
Urgent hospital admission in intensive care or burn unit.
Fluid replacement.
Temperature control.
Pain relief.
HOMOEOPATHIC MANAGEMENT-
Management plan-
Cessation of suspected medicine.
Antidoting effects of medicine-
Oversensitivity to allopathic medicines- Nux v, Sulph, Puls.
Quick reaction to allopathic medicine- Bell, Cupr, Nux-v, Zinc
Eruptions after corticosteroids, use of- Nat-m
Symptomatic medication-
Stage - blister- Bell, Cantharis, Anthracinum, Sulph.
Stage - fever - pyrogen, Acon, Bell, Bapt
Stage- ulceration– Merc, Nit ac., Ars, Lach, Sil, Suplh
Care of the lesion- Calendula, Cantharis wash and ointment in initial phase; later when ulceration occurs extra care is needed for open lesions.
NOTE- there are other “n” numbers of medicine that works wonderfully in treatment of SJS Above mentioned medicine are just for quick reference (for treating physician). Consult the nearby Physician or Hospital if you experience symptoms similar to SJS or TEN.
COMPLICATIONS-
Complications occur in severe or late diagnosis of the condition. However, in the acute phase- SEPSIS and DEHYDRATION is the major aggravating condition.
Common complications includes-
Ocular- blindness
Cutaneous- pigmentation or scarring
Mucosal - in case of ulceration or erosion- stricture and scarring may cause functional disturbances.
Organ involvement (liver, lungs, renal) may alter the functioning of the affected organ.
Recent Blog
Related Products
0 Comments